The question: “I have a hard time remembering things
and often feel exhausted, like I can’t clear my head at all. Is this
brain fog,
and is there anything I can do to fix it?”
اضافة اعلان
The blank space in your mind, when it appears, can be
confusing. What were you just saying? Did you need to pick up chicken and
carrots on your way home, or was it just the chicken? Why is it suddenly so
hard to pay attention to what you are doing, and why does it feel like your
brain is suddenly 30 years older than you are?
If you are feeling sluggish and forgetful, easily distracted
or completely overwhelmed by mundane tasks, you may be experiencing a common
phenomenon known as brain fog. Although it is not an official clinical
diagnosis that would end up in a medical chart, brain fog can arise after
several sleepless nights, while taking certain medications like antihistamines,
or as a result of jet lag — among many other scenarios. Some people experience
a form of brain fog after indulging in a big meal, during particularly
stressful periods of life, or when undergoing big hormonal changes, such as
during pregnancy or menopause.
Brain fog can also be a symptom of illness; it can occur
with
Lyme disease, lupus, and multiple sclerosis, after cancer treatment or
even during a particularly bad cold.
In recent years, the term has also become closely associated
with the cognitive impairment many people experience during or after a bout
with COVID-19. Roughly 20 percent to 30 percent of COVID-19 patients have some
brain fog that persists or develops during the three months after their initial
infection, and more than 65 percent of those with long COVID report
neurological symptoms too. “It’s becoming a neurological health crisis,” said
Dr Michelle Monje, a neurologist at Stanford University who has studied both
chemotherapy- and coronavirus-related cognitive impairment.
When should you see a doctor?
Brain fog can be frustrating and worrisome no matter when or
how you get it. The cognitive issues may wax and wane — in COVID-19-related
brain fog as well as other types, said Jacqueline Becker, a clinical
neuropsychologist at
Mount Sinai Hospital in New York. But if your symptoms
persist over several weeks or make life agonizingly difficult, you should seek
a medical evaluation.
20–30%
of COVID-19 patients have some brain fog that persists or develops during the three months after their initial infection.
“There are some people who are able to carry on with their
jobs and their regular lives, but they may need to take more frequent breaks
between tasks,” Becker said. “And then there are other people who are just
completely disabled by this.”
How is it diagnosed?
Although brain fog sounds vague and temporary, like bad
weather that will clear over time, research is beginning to show that it can
affect some people for months and take over many aspects of life, compared with
run-of-the-mill sluggishness or forgetfulness. Brain fog tends to affect
executive function — a set of skills that are essential for planning,
organizing information, following directions and multitasking, among other
things. “When executive function is impaired, it will often impact several
domains of cognitive ability,” Becker said.
Many clinicians prefer to use the term “cognitive
impairment” to lend more medical legitimacy to what patients go through, and
start the diagnostic process with cognitive exams used to measure executive
function in severe illnesses such as dementia, Becker added. The key difference
is that brain fog does not get progressively worse the way mental abilities
degenerate with dementia. You may have some days that are worse than others,
but brain fog tends to impair your cognitive function to the same extent each
time.
A variety of blood tests can also help point to some causes
of cognitive impairment, such as sleep apnea, vitamin B deficiency, or other
hormone and thyroid issues, said Dr Joanna Hellmuth, a neurologist at the
University of California, San Francisco. But because brain fog can present in
so many different ways and because it has so many different causes, the
diagnostic tests have their limitations, she added.
Sometimes brain fog may be hard to diagnose because it is
caused by several different factors, even for a patient who has one overarching
condition. Someone with lupus or multiple sclerosis, for example, may
experience cognitive impairment because of direct damage to their brain cells —
but they also may not be getting enough sleep, could have extensive fatigue or
be on medications that contribute to brain fog.
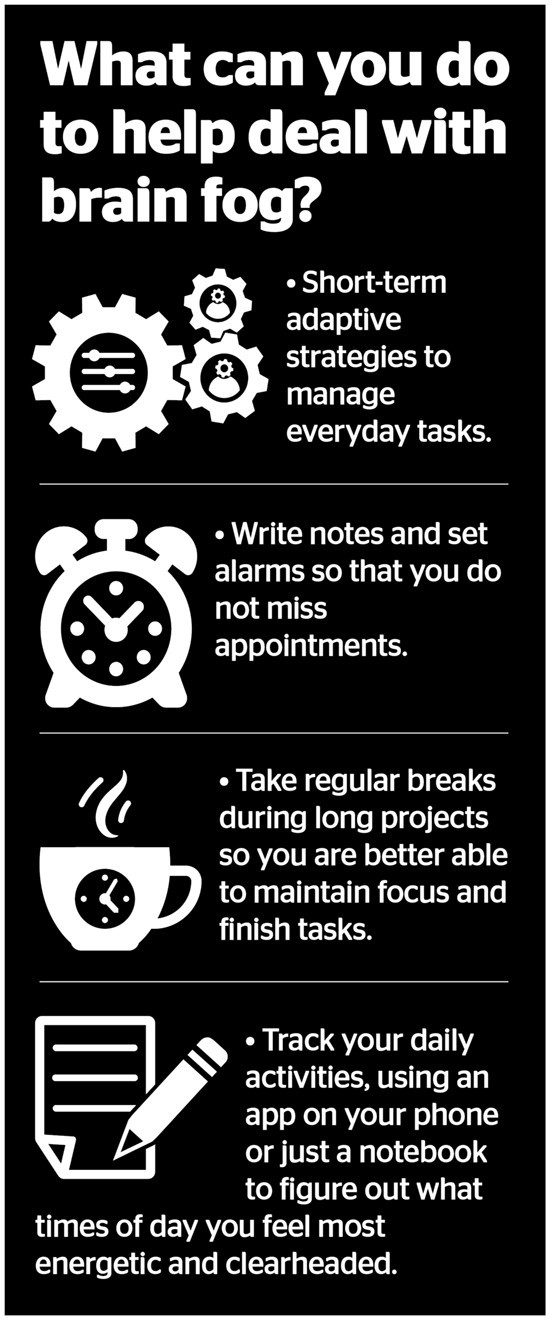
How do you clear up brain fog?
Even if doctors cannot find a physical cause for your brain
fog, there are steps you can take to manage it, Hellmuth said. Start with
short-term adaptive strategies to manage everyday tasks. Write notes and set
alarms so that you don’t miss appointments. Take regular breaks during long
projects so you’re better able to maintain focus and finish tasks. You might
also try tracking your daily activities, using an app on your phone or just a
notebook to figure out what times of day you feel most energetic and
clearheaded. Then, reserve this time to do more difficult or complicated tasks.
Your health care provider may also suggest making lifestyle
changes to improve your overall health and energy. “We try to encourage
cardiovascular exercise, a good diet, sleep, and social activities that are
known to be beneficial for the brain,” Hellmuth said.
65%
or more of those with long COVID report neurological symptoms.
Physical activity can help improve your ability to focus, as
well as increase neural connectivity and memory formation in the brain. If you
do not feel up for rigorous workouts, try doing them in small chunks so you can
slowly build up your aerobic fitness. Make sure you stay hydrated and eat a
variety of foods high in vitamins and antioxidants. And reach out to friends
and family for support. Studies have shown that maintaining a rich social
network not only helps reduce stress during difficult times, it can also
enhance intellectual stimulation and improve your brain health.
You will also want to get better rest, which, of course, is
easier said than done for patients with long COVID, those who are undergoing
chemotherapy or experiencing life changes such as pregnancy or menopause. Take
measures to relax your mind at night. Unplug your electronics and create a
restful environment.
Read more Health
Jordan News



